Chapter 4: Member Identification Cards
-
All members receive their own personal member identification (ID) card. Our New York City GHI PPO members are issued two ID cards, one from EmblemHealth and one from Anthem Blue Cross and Blue Shield (formerly known as Empire BlueCross BlueShield). Physical cards are mailed to members and are available virtually from the Member Management Eligibility look-up results in the provider portal.
A member ID card does not guarantee eligibility or payment. Providers should verify member eligibility in the secure provider portal on emblemhealth.com/providers in addition to asking to see an ID card at each visit.
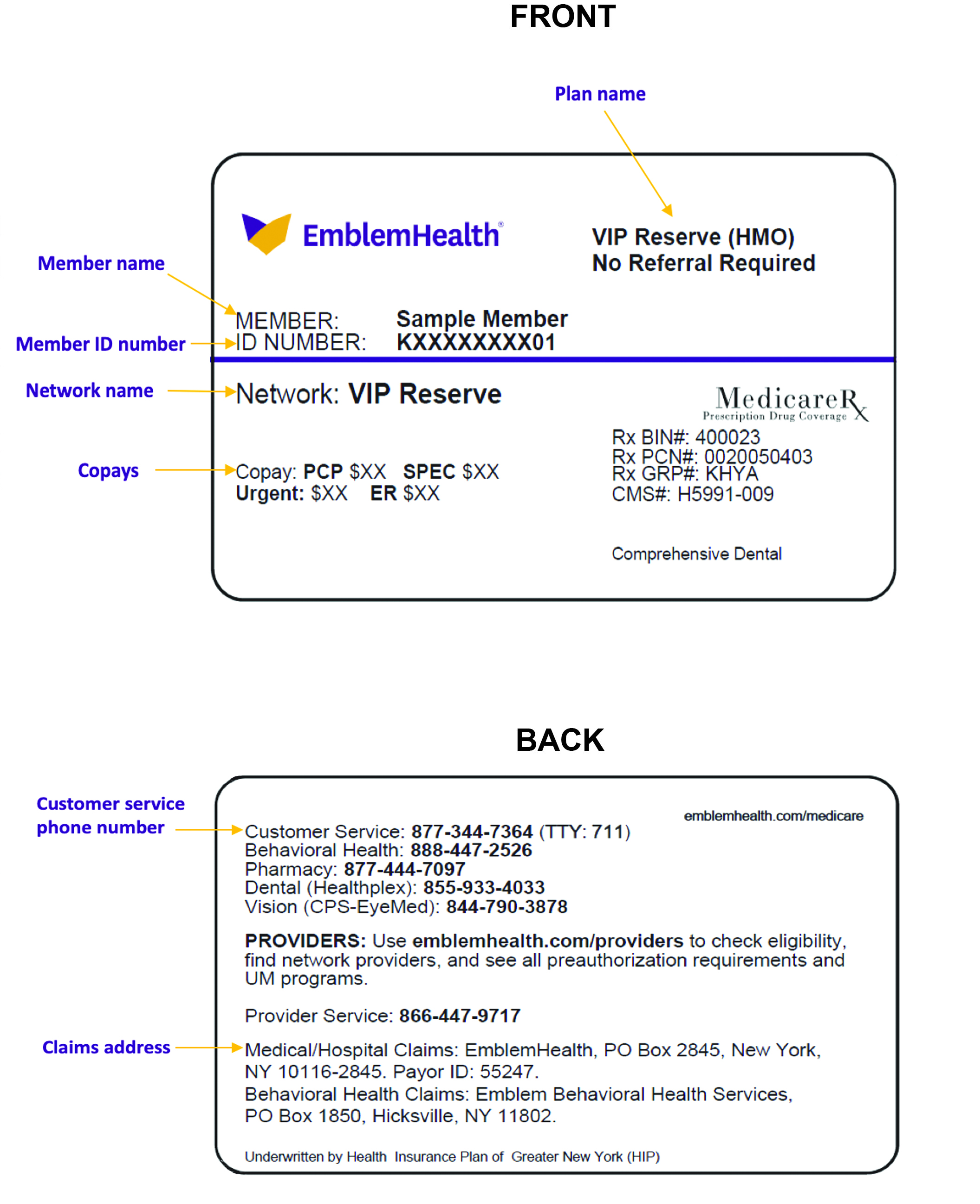
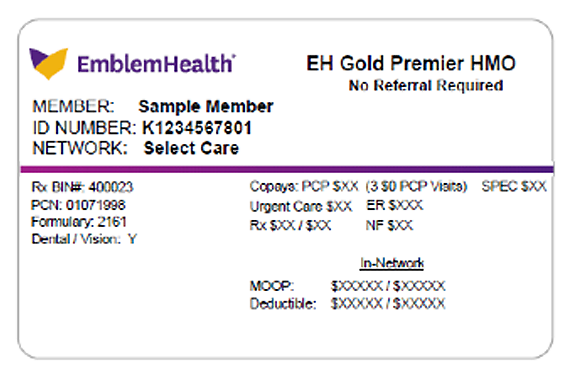
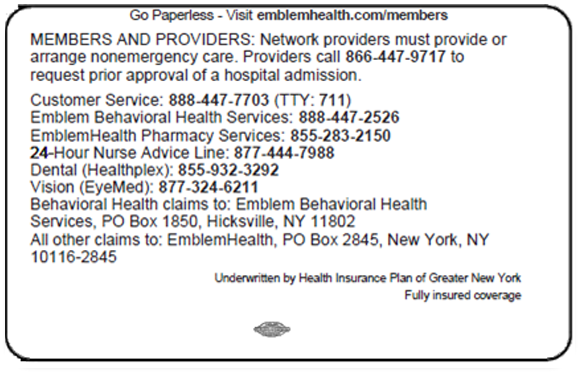
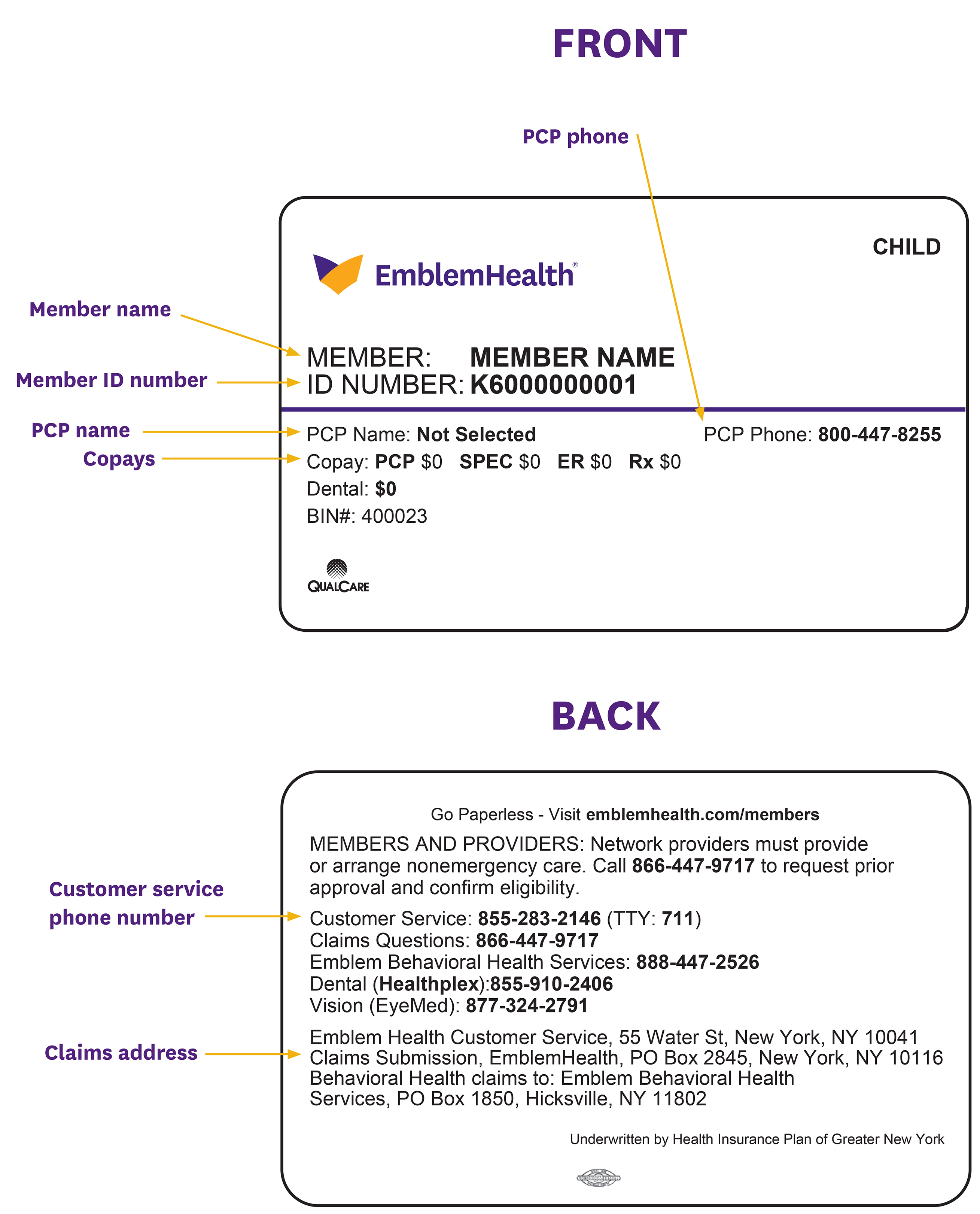
Cards show important health plan information, including the network the member may access, who is responsible for managing the member’s care, where to submit claims and ER admission/newborn notifications, covered riders, and copayments. Diagrams in the “Sample ID Cards” section of this chapter show how to quickly locate key coverage details and contact information.
-
EmblemHealth uses unique non-Social Security, number-based identification numbers. For most members, this will be an 11-digit alphanumeric member ID. The IDs start with the letter “K” followed by a unique 8-digit number (a “K-ID”). The final two digits distinguish the subscriber from each dependent (01, 02, 03, etc.). Effective January 1, 2021, EmblemHealth will issue Medicare subscribers’ dependents new unique member IDs that are not derived from the Medicare subscriber’s ID. Medicaid members receive a unique Medicaid Client Identification Number. This practice protects our members’ confidentiality and deters identity theft and fraud.
Note: GHI PPO members (other than City of New York) are migrating upon plan renewal to our new claims platform through the end of 2020. You will know a member has been migrated when you see the K-ID.
Effective July 1, 2020, GHI PPO City of New York members will use K-IDs. EmblemHealth ID cards will display the full 11 digits. Empire BCBS will adopt the same K-ID but will only use and display the first 9 digits on their member ID cards. City of New York members who are also eligible for Medicare benefits will have member ID cards issued to all family members individually in compliance with CMS regulations. Effective July 1, 2020, GHI PPO City of New York members will use K-IDs. EmblemHealth ID cards will display the full 11 digits. Empire BCBS will adopt the same K-ID but will only use and display the first 9 digits on their member ID cards. City of New York members who are also eligible for Medicare benefits will have member ID cards issued to all family members individually in compliance with CMS regulations.Remember: Please submit preauthorization requests and claims using the member ID in effect on the date of service.
-
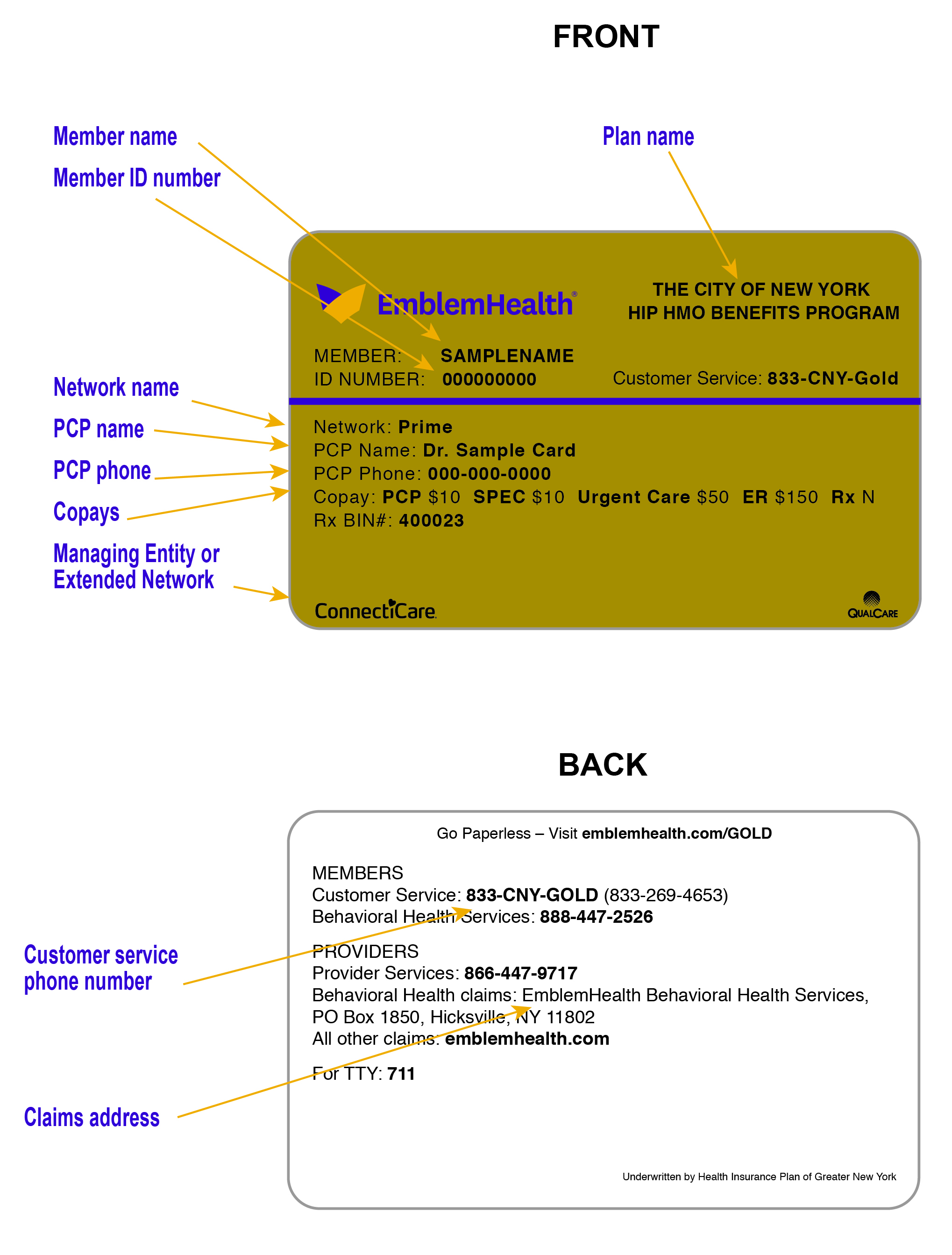
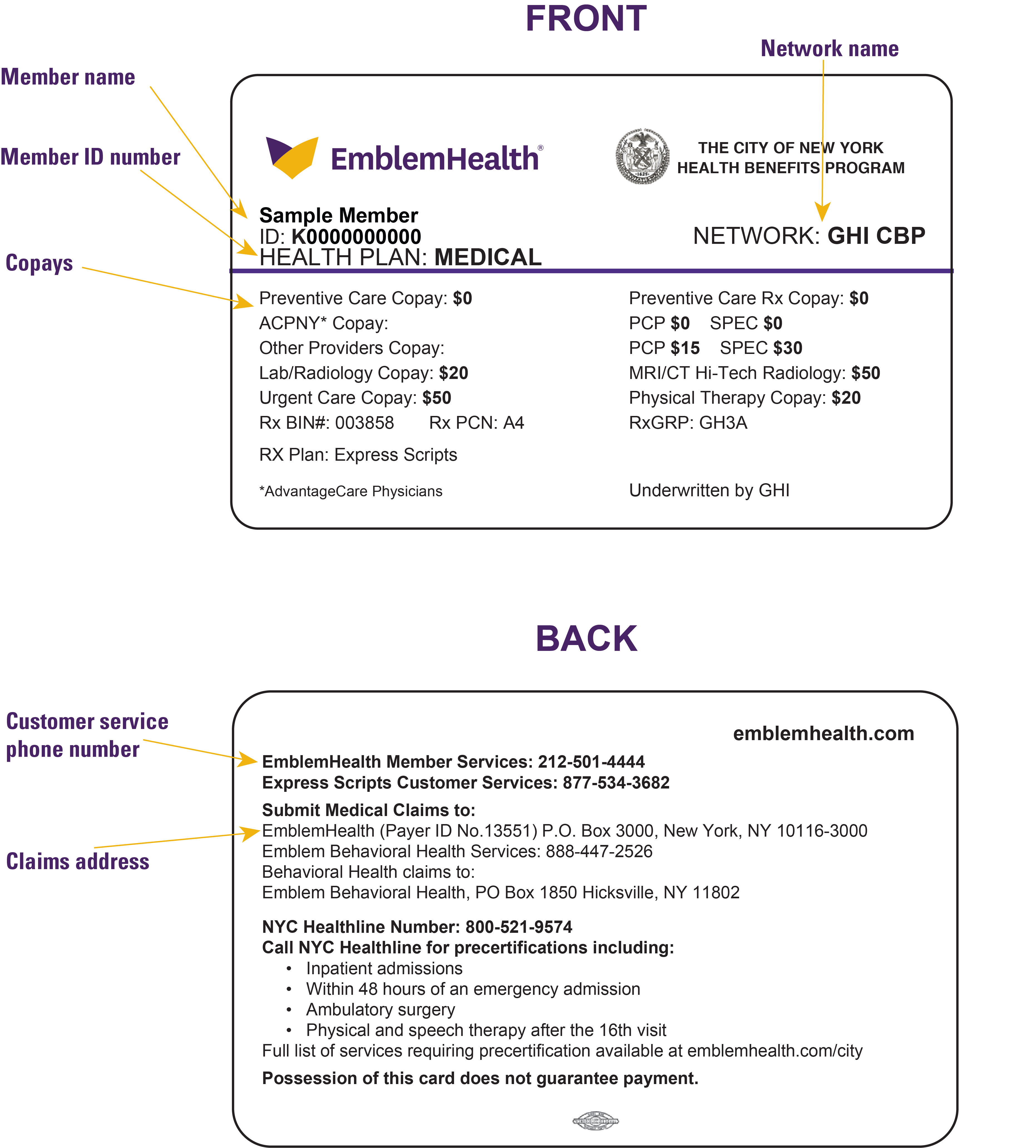
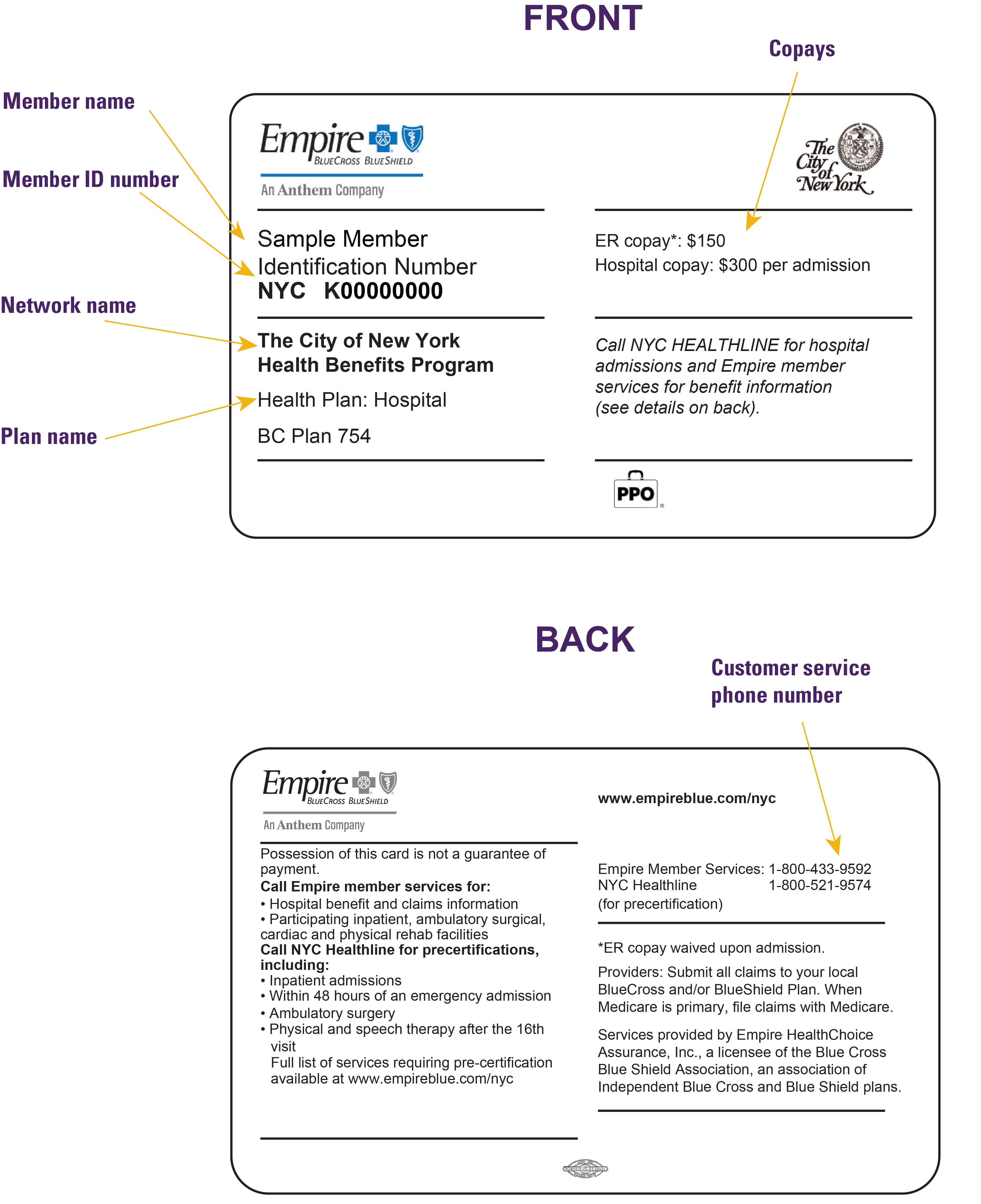
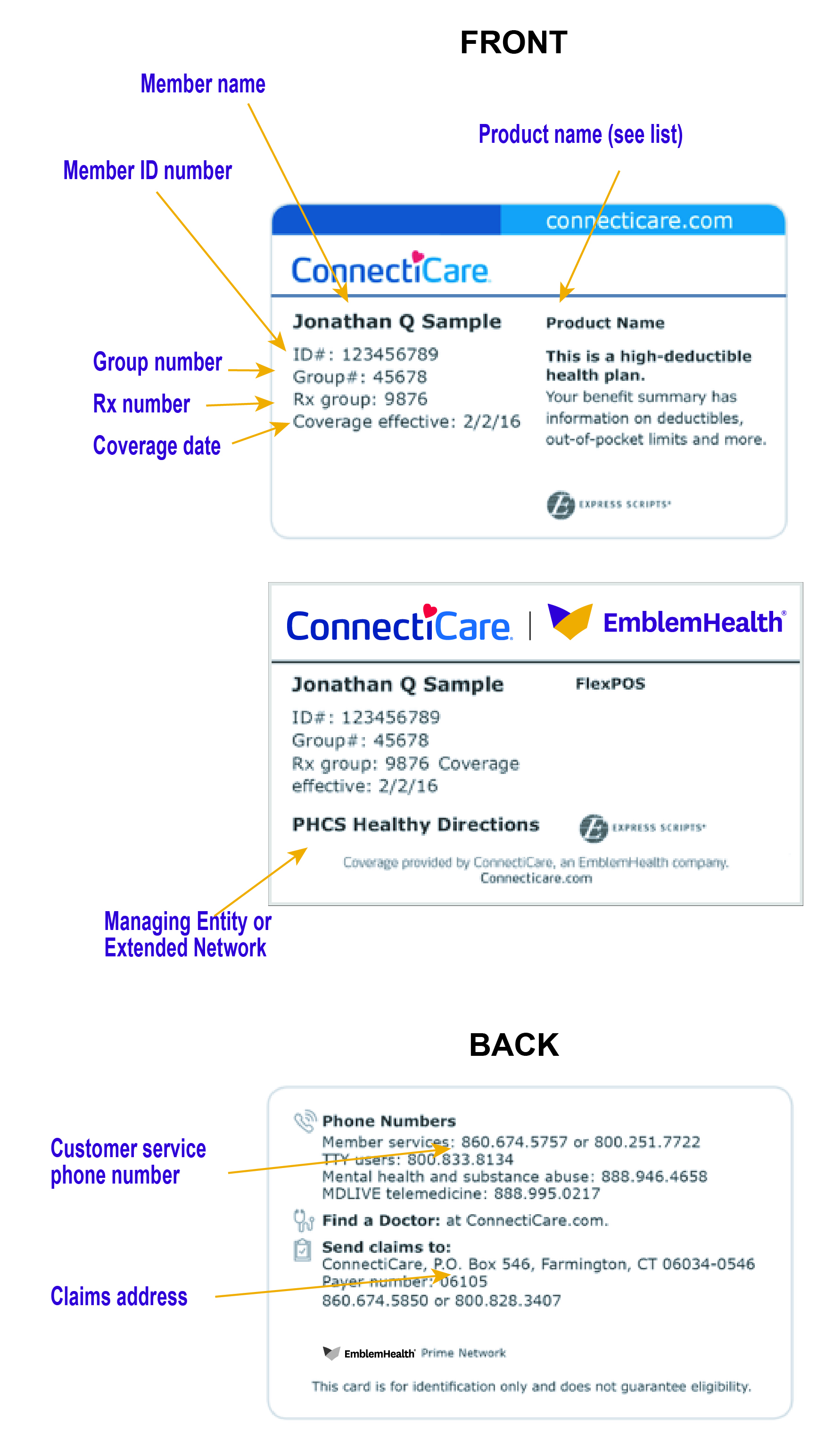
This section shows generic examples of the ID cards you may see. The diagrams point out where to find key coverage details and contact information. Actual cards will be customized based on the member’s policy.. The first section of card images shows the standard templates used for most members. The second section of card images shows the templates used for our City of New York members.
Key to Logos Used on Cards
Member ID cards may have logos for managing entities or extended networks that affect utilization management, claims submission, ER admission/newborn notification, member access to specific networks, and more. A key to these networks and entities appears below the Member ID diagrams.
SECTION 1: Standard Templates
This first two examples are the ID card templates used for most 2025 Summary of Companies, Lines of Business, Networks, and Benefit Plans and 2024 Summary of Companies, Lines of Business, Networks & Benefit Plans. These are the most common designs you will see.
The third example is the ID card template used for Child Health Plus members. Child Health Plus members access the Prime Network.
Variations of the standard templates are used for the Bridge Program. See our Bridge Program page for sample ID cards and instructions on how to use them to identify program members and the administrative processes they follow.
Section 2: City of New York ID Card Templates
The next three images are examples of the ID cards used by City of New York members. City members with a GHI PPO plan are sent two ID cards – one from EmblemHealth and the other from Empire. Both companies use the same member ID number; however, Empire adds the prefix NYC and only uses the first 9 digits of the EmblemHealth ID #, example: NYC K10000000. Please be aware of this when switching between EmblemHealth and Empire systems.
Managing Entities
HealthCare Partners: The member is assigned to an HCP primary care physician. The managing entity is responsible for utilization management, claims processing, and ER admission/newborn notifications for assigned members. Members are exempt from many of our special utilization management programs. See program descriptions to determine if HPC’s members are excluded.

SOMOS: The member is assigned to a SOMOS primary care physician. The managing entity is responsible for most utilization management, claims processing, and ER admission/newborn notifications for assigned members. SOMOS members, however, participate in EmblemHealth’s special utilization management programs.
Extended Networks
Bridge Program: Members who have the Bridge Program on their member ID cards belong to fully insured large groups and self-funded employer groups for which EmblemHealth and ConnectiCare are providing administrative services and access to five of our commercial networks (EmblemHealth Insurance Company’s (formerly HIPIC) Prime Network, EmblemHealth Plan Inc.’s (formerly GHI) National Network, ConnectiCare, Inc.’s Choice Network, QualCare Network, and First Health Network).
See our Bridge Program page for sample ID cards and instructions on how to use them.
ConnectiCare: Some members who access care through the EmblemHealth Prime Network may also access care through ConnectiCare in Connecticut. Similarly, some ConnectiCare members may access care through EmblemHealth’s Prime Network. See the Provider Networks and Member Benefit Plan chapter for applicable plan.

First Health Network: A nationwide network for members to receive in-network coverage outside of the tristate area.


PHCS/MultiPlan: Members with access to EmblemHealth Plan, Inc.’s National Network have access to PHCS/MultiPlan outside of New York.

QualCare: Certain members with access to the Prime Network also have access to QualCare’s network in New Jersey. See the Provider Networks and Member Benefit Plan chapter for applicable plans.
DIRECTORY
Chapter Summary
Member ID Numbers
Sample ID Cards




